Periodontal disease is one of the three major diseases endangering human health, as identified by the World Health Organization. This is a chronic inflammatory disease that affects the supporting structures of the teeth and mainly includes two types: gingivitis and periodontitis. Gingivitis is typically the initial stage of periodontal disease, mainly characterized by red, swollen and bleeding gums. If not treated, it may lead to periodontitis, which can cause further damage to the tissues around the teeth. Periodontitis destroys the supporting structures of the teeth and often causes damage to the alveolar bone, leading to the loosening and losing of teeth. Due to the limited application of biofunctional materials and the existence of oral inflammation and bacterial microenvironments, it is difficult for the periodontal bone regeneration materials or technologies widely used in clinical practice to achieve alveolar bone regeneration, which is the new challenges for tooth restoration.
Based on this, researchers from Stomatological Hospital, Southern Medical University and Shenzhen Bay Laboratory designed a 3D-printed bioink for periodontitis-derived bone defect repair. The relevant research results were published in Biofabrication in an article titled “3D-printed bioink loading with stem cells and cellular vesicles for periodontitis-derived bone defect repair”.
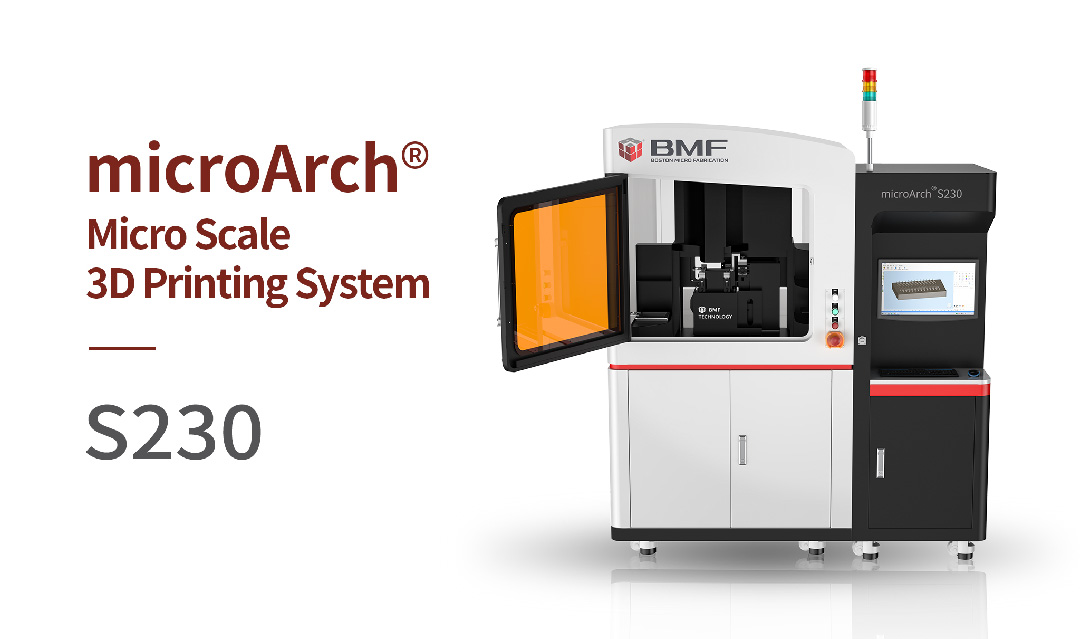
In the study, the team used BMF microArch® S230 (2μm) to print an EPLGMA-based biomimetic template. By dropping GMA into an EPL solution and irradiating it with blue light, a cross-linked hydrogel was formed. Next, PDLSCs and MDSCs membrane vesicles derived from (MDSCs-MV) from the periodontal membrane of deciduous teeth were added to EPLGMA to prepare the bio-ink. This 3D bio-ink has a reticulated porous structure that promotes cell proliferation, migration, and the exchange of nutrients and metabolites.

To evaluate the osteogenic ability of this 3D bio-ink, the researchers constructed a SD rat jaw bone defect model and validated it under simulated inflammatory conditions. After three months of treatment, the EPM@Pg group showed the best antibacterial, anti-inflammatory, and osteogenic effects.
In summary, this research has successfully developed a novel, personalized, multifunctional 3D-printed module for the treatment of periodontitis-derived bone defects. This new material not only has the natural antibacterial properties of EPL, but also performs well in anti-inflammatory response and bone regeneration, and will provide a promising new solution for the treatment of periodontitis.
Please refer to the link below to access more information about this research:
https://doi.org/10.1088/1758-5090/ad2081
BMF team has established numerous partnerships with scientific research groups and research institutes. We are eager to exchange insights with more experts and specialists to push the boundaries of science and technology. If you have any other ideas, please feel free to contact us.

